Introduction to Tardive Dyskinesia (TD)
Tardive Dyskinesia Treatment Guidelines (TD) is one of those conditions that can sneak up after long-term use of certain psychiatric or gastrointestinal medications, especially those that block dopamine receptors. It’s a movement disorder that causes repetitive, involuntary movements—like grimacing, tongue flicking, or rapid blinking—that can seriously affect a person’s confidence and quality of life. Despite its physical nature, TD is rooted deeply in the brain’s neurochemistry, which makes managing and treating it both challenging and crucial.
The tricky thing about TD is that it doesn’t always show up right away. Symptoms may emerge months or even years after starting medications such as antipsychotics. This delayed onset often leads to frustration for patients and clinicians alike, as early signs can be subtle or mistaken for something else. The condition doesn’t always reverse on its own, which is why following structured treatment guidelines is essential for managing it effectively.
Over the years, medical experts have refined approaches to TD management. Treatment is no longer about just stopping the offending drug—it’s now a strategic, multi-layered plan involving medication adjustments, targeted therapies, and patient-centered care. Let’s explore the current Tardive Dyskinesia treatment guidelines in detail and understand how experts navigate this complex disorder.
Identifying and Diagnosing TD Early
One of the most Tardive Dyskinesia Treatment Guidelines steps in TD management is recognizing the condition as early as possible. Many patients who develop TD are taking medications like antipsychotics, metoclopramide, or other dopamine receptor blockers. Because these drugs are often essential for managing psychiatric conditions, it’s not always possible—or safe—to discontinue them abruptly. That’s why early screening and monitoring play such a critical role.
Clinicians typically use standardized assessment tools such as the Abnormal Involuntary Movement Scale (AIMS) to monitor for signs of TD. The AIMS test helps quantify movement severity and track changes over time. It’s recommended that healthcare providers perform regular assessments—every 3 to 6 months for patients on long-term dopamine-blocking medications. This proactive approach allows for early detection before the movements become severe or irreversible.
Moreover, doctors must Tardive Dyskinesia Treatment Guidelines TD from other movement disorders like Parkinsonism or akathisia. This is essential because treatment strategies differ greatly depending on the underlying cause. Accurate diagnosis requires both clinical observation and a thorough review of medication history. Catching TD early provides the best chance for successful symptom management and possible reversal.
Reviewing and Adjusting the Causative Medication
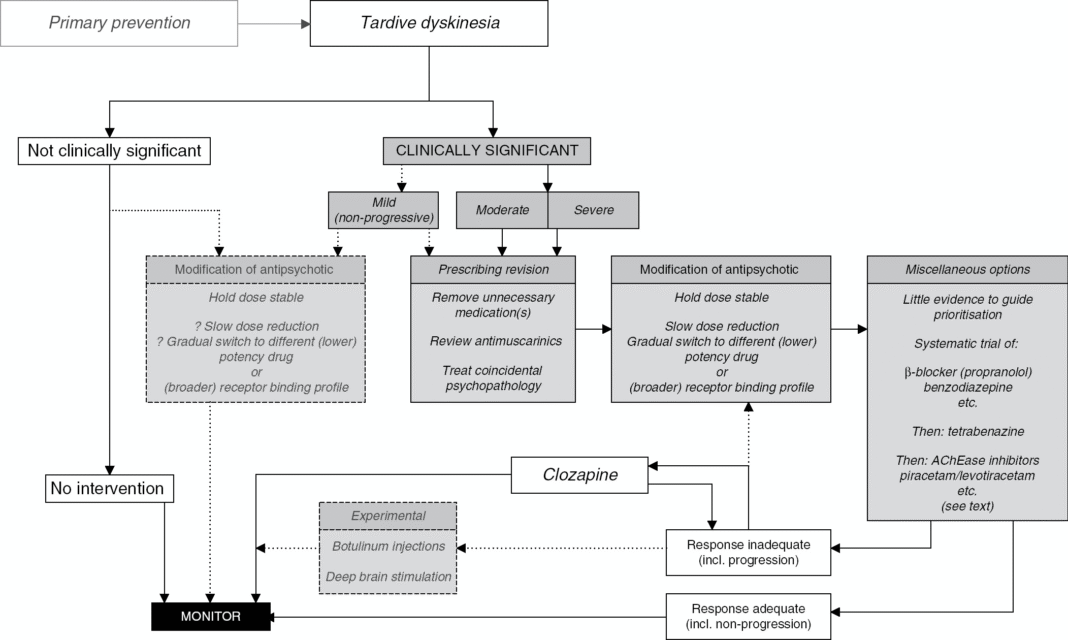
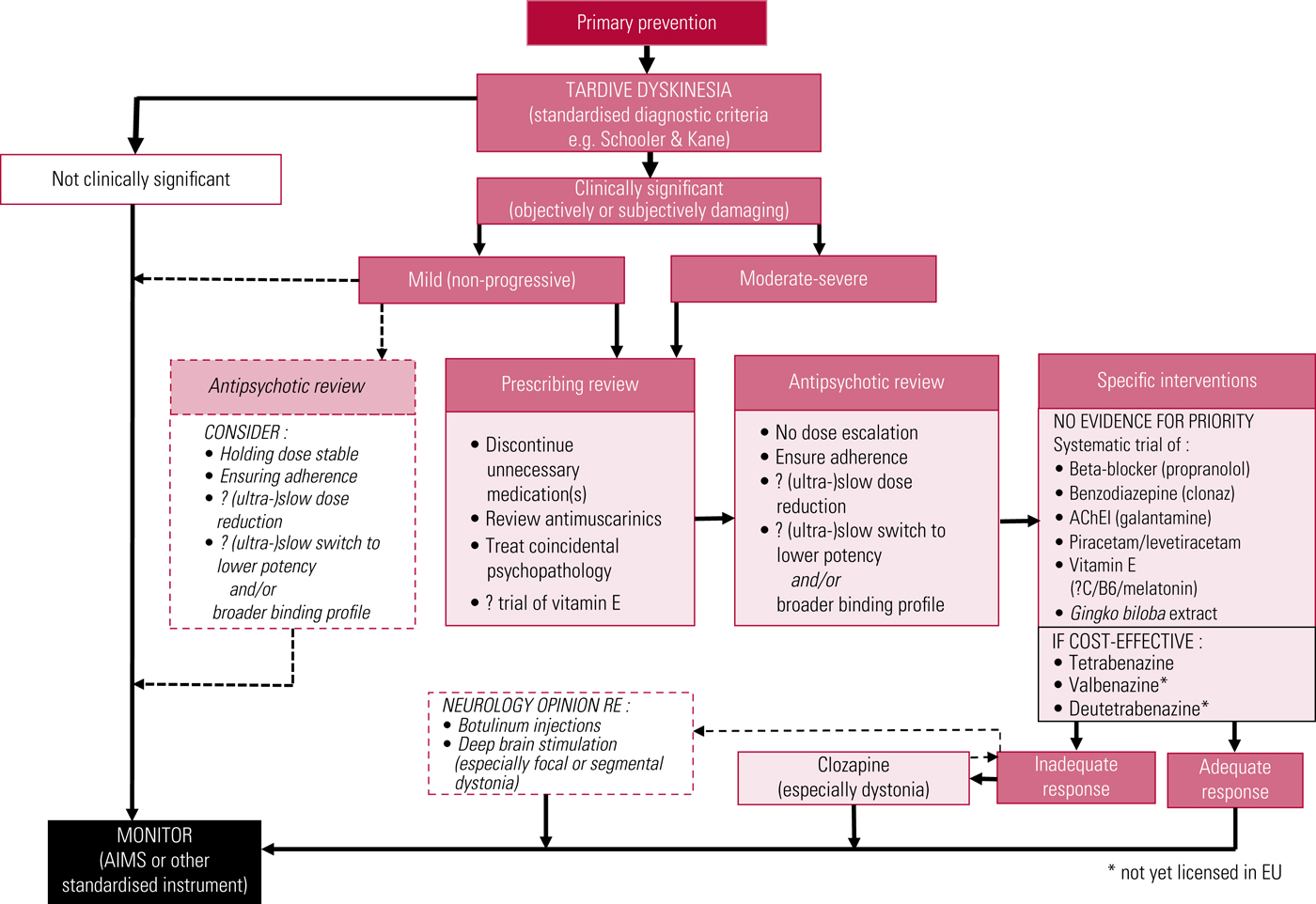
Once TD is Tardive Dyskinesia Treatment Guidelines , the first step in treatment guidelines is to review the patient’s medication regimen. Since TD is typically caused by dopamine receptor–blocking agents, adjusting or discontinuing the offending drug is often the initial intervention. However, this process must be handled carefully, especially for individuals with schizophrenia, bipolar disorder, or major depression, where antipsychotics are vital for stability.
If possible, clinicians may attempt to reduce the dose of the causative medication. In some cases, switching from a first-generation (typical) antipsychotic to a second-generation (atypical) one—such as quetiapine or clozapine—can help lower TD risk while maintaining psychiatric control. Clozapine, in particular, is known for having the lowest risk of causing or worsening TD and may even improve symptoms in certain cases.
However, sudden withdrawal of Tardive Dyskinesia Treatment Guidelines is not recommended, as it can trigger severe relapses of psychiatric symptoms. The adjustment must be gradual and monitored closely. The goal is to find a balance—reducing TD symptoms while keeping the underlying mental health condition well-managed. Each decision must be individualized, considering both the benefits and potential risks for the patient.
Pharmacologic Treatments for TD
The introduction of specialized medications has revolutionized TD management in recent years. Two FDA-approved drugs—valbenazine (Ingrezza) and deutetrabenazine (Austedo)—have become the cornerstone of pharmacologic treatment. These medications are vesicular monoamine transporter 2 (VMAT2) inhibitors, which work by regulating dopamine release in the brain, thereby reducing abnormal movements without causing major psychiatric side effects.
Valbenazine is typically taken once daily and has shown remarkable efficacy in reducing TD symptoms over time. Clinical trials have demonstrated significant improvements in AIMS scores and overall motor function. Similarly, deutetrabenazine, which is structurally related to tetrabenazine but has fewer side effects, offers flexible dosing and excellent tolerability. Both medications have been proven effective across different patient populations, making them first-line treatment options according to modern guidelines.
Beyond VMAT2 Tardive Dyskinesia Treatment Guidelines , other drugs may be used off-label depending on the case. For example, clonazepam (a benzodiazepine) or ginkgo biloba extract have shown mild benefits in some studies. However, these alternatives are generally considered secondary options. The priority remains VMAT2 inhibitors due to their evidence-based success in reducing involuntary movements safely and sustainably.
Non-Pharmacological and Supportive Therapies
While Tardive Dyskinesia Treatment Guidelines plays a leading role in TD treatment, non-pharmacological strategies also make a significant impact. Supportive therapies focus on improving daily functioning, emotional well-being, and overall quality of life. For many patients, living with visible involuntary movements can be socially isolating and psychologically distressing, so therapy and education are key components of care.
Behavioral therapy and occupational therapy can help patients adapt to their symptoms, develop coping mechanisms, and maintain independence. Speech therapy may also be beneficial for those experiencing facial or tongue-related movements that interfere with communication or eating. These interventions aim to help patients manage symptoms in practical, meaningful ways.
Additionally, patient education is a cTardive Dyskinesia Treatment Guidelines ornerstone of TD management. Understanding what causes TD, how it’s treated, and what can make it worse empowers patients to take an active role in their care. Support groups and counseling also help individuals process the emotional toll of the disorder. When combined with medical management, these supportive therapies create a more comprehensive treatment approach that addresses both the physical and emotional aspects of TD.
Monitoring Progress and Long-Term Management
TD Tardive Dyskinesia Treatment Guidelines isn’t a “one and done” process—it’s a long-term commitment that requires ongoing monitoring. Regular follow-ups allow healthcare providers to track symptom progression, evaluate medication effectiveness, and make timely adjustments. The AIMS test remains the go-to assessment tool for this purpose, helping clinicians document changes over time and respond accordingly.
Since VMAT2 inhibitors don’t cure TD but rather manage symptoms, continued use is often necessary to maintain results. That’s why patient adherence is critical. Missing doses or discontinuing treatment prematurely Tardive Dyskinesia Treatment Guidelines lead to symptom recurrence or worsening. Patients should be encouraged to communicate openly about side effects or changes in movement patterns so that their regimen can be fine-tuned for optimal comfort and control.
Another important consideration in long-term management is comorbid conditions. Many TD patients also live with mental health disorders that require ongoing therapy. Integrating psychiatric care with TD treatment ensures that one area of health isn’t sacrificed for the other. Collaborative care—between psychiatrists, neurologists, and primary care providers—is considered best practice for maintaining both Tardive Dyskinesia Treatment Guidelines stability and motor control.
Emerging Research and Future Directions
The field of TD research is evolving rapidly. Scientists are exploring new ways to not just manage symptoms but also address the underlying neurochemical imbalance that causes TD in the first place. Studies are focusing on neuroprotective agents, anti-inflammatory compounds, and even gene-targeted therapies that could prevent TD from developing at all.
Another promising area involves early intervention protocols, which aim to detect subtle movement abnormalities before they fully develop into TD. With advances in wearable technology and AI-assisted motion analysis, clinicians may soon be able to identify early warning signs that are invisible to the naked eye. This could completely change how TD is diagnosed and managed in clinical settings.
Ultimately, the goal of future treatment guidelines will be prevention. By Tardive Dyskinesia Treatment Guidelines safer psychiatric medications and refining patient monitoring strategies, the hope is that TD will one day become a preventable rather than lifelong condition. Until then, following current evidence-based guidelines remains the best way to manage symptoms and improve quality of life for those affected.
Conclusion: The Path to Better TD Management
Tardive Dyskinesia Treatment Guidelines can be a daunting condition to live with, but modern treatment guidelines have made it far more manageable than in decades past. From early detection and medication adjustments to advanced pharmacologic options and supportive therapies, patients now have multiple avenues for relief.
The key lies in collaboration—between patient and provider, and between medical disciplines. With ongoing research and personalized care, individuals with TD can lead fulfilling lives while minimizing the impact of their symptoms.
If you or someone you know is taking dopamine-Tardive Dyskinesia Treatment Guidelines medications, stay proactive. Regular screenings and open communication with your healthcare provider are your best defenses. Tardive Dyskinesia doesn’t define a person—it’s a challenge that, with the right strategy, can absolutely be managed with confidence and care.